John Gurdon of Cambridge University and Shinya Yamanaka of Kyoto University received the 2009 Albert Lasker Basic Medical Research Award for discoveries concerning nuclear reprogramming, the process that instructs specialized adult cells to form early stem cells — creating the potential to become any type of mature cell for experimental or therapeutic purposes.

Gurdon, who at 76 has much better hair than Yamanaka (47), will share with him a prize that is usually seen as a lead up to a Nobel Prize (In the 63-year history of the Lasker prizes, 76 winners also have won a Nobel).
[Read the Lasker Foundation official award justification
here]
Gurdon was the first to overturn conventional wisdom by showing that cell development isn’t always a one-way process in which cells go from embryo cells, able to become any other cell type, to unchangeable cells like muscle or nerve cells.
“The prevailing thought was that as cell differentiate, they lose their ability to generate other cells of any kind,” Gurdon told
Bloomberg. Gurdon took cells from an adult frog’s gut, inserted the nucleus into an egg cell whose own nucleus had been removed, and created a tadpole with the genetic characteristics of the original frog. His work showed that the adult cells retained the ability to become other cells and that the egg had the power to reawaken those properties.
More than four decades later, Shinya Yamanaka showed that the same results could be achieved without the use of eggs. In 2006, Yamanaka introduced four genes — Oct3/4, Sox2, c-Myc, and Kif4 — into mouse skin cells to transform them into induced pluripotent stem cells —he called them “iPS” cells— which were almost indistinguishable from embryonic stem cells.
“We did it by transferring the nucleus of a cell,” Gurdon said. “Amazingly, he does it by adding genes to the cells and some of them go back to being embryo cells.” "I did not expect it would be possible to do what Yamanaka did.”
The next year Yamanaka published the seminal human iPS paper using the same genes to achieve pluripotency in fibroblast cells:

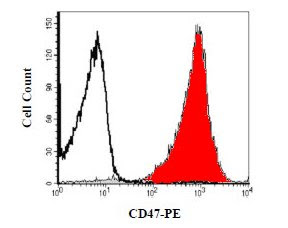
R&D Systems reagents used in this study: